Blog
Explore bold perspectives
Our team enthusiastically discusses the latest tech, UX trends, and health industry topics. We want to open those discussions to you! Check out our latest bold insights and join the conversation.

Human factors optimization: How to leverage HF researchers in your medtech team
As a medtech professional, you can enhance your team’s capabilities by engaging human factors researchers to create front-end documentation, alleviate research workloads, and provide regulatory guidance.

Enhancing medical device safety and effectiveness: Leveraging knowledge tasks in healthcare UX and human factors research
Discover why implementing knowledge tasks is essential for evaluating user comprehension of critical safety information in medical device validation. Learn how to effectively assess these tasks to enhance product safety and effectiveness in your healthcare UX research.
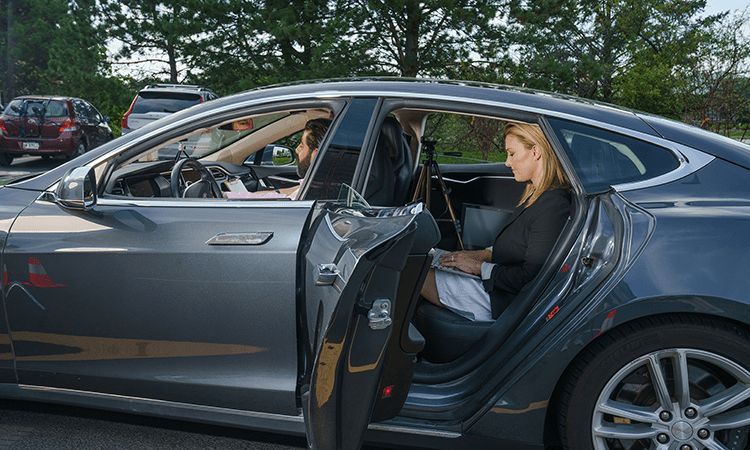
3 considerations for accessible in-car UX research sessions
Adaptability, alternative setup options, and a prioritized task list are all helpful components to planning in-car research studies for populations with accessibility needs.

Integrating AI with care: FDA reveals focus areas for forthcoming guidance on AI products
As AI technology use expands within the healthcare industry, FDA focus areas will play an important role in ensuring safe implementation.

Fostering collaboration between HF practitioners and interdisciplinary teams
Discover how integrating human factors expertise drives success in product design and learn the steps to foster collaboration through interdisciplinary teamwork.

Harnessing UX research to empower children and enhance parental controls online
As the UK rolls out its Online Safety Act, platforms must improve their parental control systems. Read on to discover how UX research can shed light on the complexities of effective parental controls, enabling designs that empower parents and protect children online.

Revolutionising women’s health: The power of Femtech and inclusive design
On this International Women’s Day, we advocate for user-centered design of Femtech solutions to address diverse needs in women’s health.
Follow this framework to ensure your SaMD conforms to HF standards post-release
Navigate regulatory nuances for your SaMD by following a structured approach to maintain compliance post-release.

AI Governance: Safeguarding innovation in an evolving regulatory landscape
Discover how leading experts at CES 2024 navigated the complex landscape of AI innovation and risk governance, offering invaluable insights into launching AI products responsibly amidst evolving regulations.

Decoding the user experience of conversational AI
Our CUI expert discusses the complexities of evaluating and improving UX in conversational AI, focusing on factors like personality, context, and conversation flow.

GenAI at the inflection point: Navigating the third wave
2024 is forecasted to be a crucial inflection point for AI, marking the third wave of transformative technologies. Here, we break down learnings on GenAI from our visit to the Consumer Electronics Show.

So you want to run a diary study: Five steps to successfully onboard participants
Successful participant onboarding is a crucial step in running a diary study. Read on for five steps for effective onboarding: establishing processes, internal testing, progress tracking, time allocation, and consideration of global factors.

The role of AI in transforming the car-buying experience
Insights from CES 2024 highlight AI-driven changes in the automotive sales experience: customer-centric strategies, opportunities for personalization, and evolving business models reshaping the industry.

The future of automotive infotainment: Connect the dots for an immersive experience
At the 2024 CES, it was clear the demand for an unparalleled in-car experience is igniting a revolution, reshaping the way humans perceive and interact with vehicles. We gathered 6 takeaways from the conference for delivering the next gen experience in auto infotainment.

The value of the daily fieldwork debrief: A critical piece of your UX research
A summary of the day’s research findings helps teams to stay aligned, drives report outcomes, and ensures stakeholder goals are top of mind.

Context, accents, and privacy: Overcoming hurdles of AI translation tools in global UX research
Bold Insight launched a global AI study in March 2023 that included: 24 multilingual interviews conducted with UX researchers in 19 countries, spanning 22 languages. 27 interviews in English with global UX researchers representing 24 countries. Our global study led us...

The role and challenges of speech technology in global UX research
Speech technology helps UX researchers bridge linguistic and cultural barriers. Effective use, however, depends on balancing the roles of humans and tech.

Generative AI in UX research: what are the risks and rewards?
Generative AI can speed up repetitive research tasks, but it’s still hard to trust each output. Our global AI study measures the concrete impact.

Lost in translation: Challenges second-language speakers face when using voice interfaces
Research uncovers the needs and challenges faced by bilingual individuals when interacting with smart speakers, offering valuable insights for improving conversational technologies.

What medtech design teams need to know about AI regulations
China and the European Union are regulating AI ethics. The mandate for medtech design teams: build AI-powered products that meet ethics standards and inspire user trust.

How to show up for your participants and colleagues this Pride Month and beyond
This Pride Month, feel encouraged to step up for your colleagues, your participants, and your clients by recognizing the importance of gender and sexuality diversity.

Conducting research with kids? Considerations for running studies with adolescent participants
Unlock valuable insights by creating engaging environments, maximizing participation, and uncovering the genuine perspectives of young users.

Want to increase employee retention? Design your company around your employees
We designed Bold Insight to deliver our employees’ best work. The result: a workplace that reflects the emotions, ideas, and experiences of all our employees.

Why employee experience should get the same attention as user experience
Employees are a key user group at any organization. Applying UX research principles can help HR leaders optimize employee experience, drive engagement, and boost the bottom line.

Designing for accessibility? 6 considerations for a more inclusive user experience
Insights from conducting UX research can help put your product on the map when it comes to ensuring accessibility for all users.

Not sure how to use AI tools in your UX research? Consider making it your sparring partner
Generative AI can help researchers refine and clarify research objectives, communicate effectively, and spark creativity and strategic thinking.

3 crucial aspects of submitting a successful human factors engineering package to the FDA
Regulations and guidance for human factors research and medtech have evolved, but the goals remain unchanged. The right research partner makes navigating FDA rules simple.

A voice for everyone: Embracing diversity in speech technology
The technology behind voice assistants continues to improve, but further changes can be made to better accommodate a broader range of speakers and to design for a more inclusive future.

How collaboration builds value in medical device human factors research
Instead of a top-down, one-size-fits-all approach to research, collaboration between manufacturers and human factors research teams can create trusted partnerships and a focus on designing valuable products.

The UX of mental health: 5 considerations when designing a mental health app
Ease of use, data privacy and personalisation are just a few of the considerations to keep in mind when developing the user experience of a mental health app.

4 make-or-break considerations for health IoT ecosystems
To boost adoption of IoT devices, medical device manufacturers should consider four key questions to gain insights into user contexts and perceptions.

10 tips to better support a11y participants during user research
With a few considerations and thoughtful planning, research that includes the a11y community can effectively collect data while ensuring a respectful participant experience to help design products that meet the needs of all users.

5 tips for remote UX research with the A11y community
By being thoughtful of the research process and unique needs of participants, researchers can champion inclusion of those with accessibility needs in research, resulting in better designed products.

Six unique benefits of rolling research
Consider rolling research for increased efficiency and continuity in your product development process.

How can UX researchers support gender diversity and more inclusive design for all intended users?
Update research and design practices to increase gender diversity; data from research that encompasses all genders is more reflective of real-world users.

The secret communication weapon everybody forgets about in 2022
Don’t overlook the telephone in your search for simple, effective methods to promote seamless communication in your dispersed workforce.

Understanding user research regulations: how much do you know about participant privacy?
Choose an experienced research partner to avoid privacy pitfalls that can derail successful data collection.

Why and how your company should talk about pronouns
Encourage a welcoming and inclusive environment by including pronouns more naturally in your interactions.

Ten questions workforce leaders should be ready to tackle with the Omicron-fueled COVID case climb
Clear and immediate communication with your workforce is the key to improving employee experience during and beyond the latest COVID surge.

Why logistics are important: 4 considerations for planning global research
A successful global project starts with understanding and planning for logistical challenges.

Two tips for successfully preparing research materials for global studies
Prepare for a successful global study by allocating additional time to strategize localization and translation.

How to prepare products for global research
Understanding and accounting for common challenges is the first step in collecting high quality data during global research.

Four ways the pandemic has permanently changed UX research
Data suggests the COVID 19 pandemic increased demand for UX research and contributed to skill growth among researchers.

Support a company culture of self-advocacy with these four tips
Uncover insights to encourage a self-advocacy culture with authentic employee engagement.
Improve medical device safety with these packaging design tips
Safe and effective medical device use starts with designing packaging that considers the unique needs of its users.

Moderating remote research sessions? 3 tips to help build rapport with participants
Gathering quality data during remote sessions begins with ensuring participants are equally as comfortable as they would be during an in-person session.

3 tips to successfully onboard in a remote environment
A focus on building connections and involvement with remote co-workers is key in both successful onboarding for new employees as well as employee retention.

Reflecting on an unprecedented year with mixed emotions
With optimism, we reflect on a year of new challenges as we await the return of our ‘old’ normal.

Ageism and technology UX: Designing for seniors
It’s time for tech companies to turn their attention to designing solutions for a senior community that is more in need of connection than ever before.

5 tips to mitigate use-related risk for pre-filled syringes and other injection devices
Attention to logistics, thoughtful product and research study design, and iterative user testing can help mitigate use-related risk with injection devices.

It’s coming to your website! UX will factor into Google search rankings
Create a better website experience for your customers and improve your search visibility with insights gained through remote moderated testing.

Working from home: Tips for designing your workspace from an ergonomics expert
Remember “right angles” to ensure your home workspace is designed for productivity and comfort

New Blog Series: Bold Insight and Orthogonal share insights about getting medical devices to market faster
Given the multidisciplinary nature of MedTech and connected health, we have the opportunity to work with a wide variety of professionals including engineers of many stripes, scientists, researchers, designers, experts in regulatory, and quality management. Our...

Rethinking experiences: UX and human factors research can help companies develop safe, contactless designs
Explore early opportunities to create and refine a truly functional contactless experience for your customers, addressing new expectations in a changing world.

Remote UX research can reveal 5 key insights for auto manufacturers
When in-person testing is not feasible, stay on track by using remote interviews to collect data and refine the in-vehicle experience for your consumers.

Will participants show for fieldwork?
Promising numbers indicate that with safety precautions, participants are willing to return to in-person research.

Webisode: Possible impact if in-person human factors research is not considered essential
Conducting research to inform development of safe and effective medical devices is essential and with modifications and precautions, in-person research can be conducted safely and effectively.

Now is the ideal time to improve the UX of your mobile app
As the demand for app-based services grows, now may be the time to invest in UX research to identify needed improvements and enhancements.

Human factors research in the times of COVID
Human factors research in the support of medical and drug delivery device commercialization is essential and we should be planning on a return to in-person research as soon as is possible by applying all available and practical protective measures.

COVID-19: Using human factors and UX to make a positive impact
We have aggregated some considerations for HCPs, healthcare organizations, and others involved in the medical space.

Is FMEA inadequate for human factors analyses?
A “traditional” risk assessment does not meet the needs of FDA-required human factors analyses.

Pros and cons of remote moderated testing: Considerations for ongoing research during COVID-19
A few key adjustments can help capture research data effectively and ensure the health of participants and team members.

What we do matters: A Bold mission
We are focused on doing what’s right for our clients, our employees, our company, and our world.

Be the student: 4 tips to be a better UX research moderator
Moderators should put themselves in the position of learning from the participant. Keeping a few tips in mind can facilitate this process and produce a more fruitful UX research session.

Care to share? UX considerations of the sharing economy for ridesharing, hospitality, and healthcare
The sharing economy, primarily based in digital platforms, is poised for companies to stand out by delivering exceptional user experiences.

UX research reveals common concerns from HCPs about telehealth technology
Our research has shown a trend in healthcare provider feedback regarding mHealth alerts and features. While generally positive about the concept, liability is top of mind with this user group and common questions were raised during testing.

So, your recruit fell apart… now what?
With the thousands of projects managed over the years, we feel like we’ve “seen it all.” While rare, in spite of the amount of preparation and planning, sometimes things don’t go as expected.

7 insights from the 2019 HFES Health Care Symposium
HFES healthcare symposium provides insight on FDA and regulatory perspectives, use of technology in research, interesting research methods employed, and cross-industry collaboration.

Product design: Why it’s important to see behavior
As designers, we assume users will behave the way we expect them to behave. Unfortunately for us, humans are unpredictable … attempts to model behavior typically predict less than 10% of actions. Consider the Theory of Planned Behavior, which suggests behaviors depend...

Is a product still usable if the user has to “get used to it?”
Does a user’s inability to successfully “walk up and use” a product necessarily point to usability issues?

Research shows big payoff when design includes voice of the user
A recent McKinsey report outlines the ROI of UX research, offering a business case to invest in building designs centered around the user.

6 UX trends for 2019
As industries undergo massive change, there’s a tension; new players will disrupt old market structures and the UX is going to play a critical if not defining the role in the success or failure of these transformations.

A Bold year to remember!
Guided by 20 years of experience, we are dedicated to using what we’ve learned to benefit our clients, empower our employees, and give back to our community.

Four things to keep in mind when conducting on-the-road UX research
To successfully execute on-the-road driver experience research, it’s important to account for factors unique to the driving environment, such as the route or geographic location.

When building next gen fintech, start with research in Africa
The user experience (UX) of emerging FinTech might be considered superior in Africa compared to the United States. In Africa, the utility of cryptocurrencies has been communicated and made known, effectively improving the UX of this emerging technology.

When it comes to voice print UX, what is our role as researchers?
During a recent study, we asked participants how long they thought they would have to speak in order for their voice to be uniquely recognized (i.e., voice print). While their estimates varied widely - from 30 seconds to 30 minutes - most people said about three to...

Is customer channel-hopping hiding UX problems?
Listen to reasons customers contact you and use those reasons to diagnose problems in your channels that may be hiding.

UX principles for robot design: Have we begun to baseline?
As the robotics industry continues to find its way into our lives, we can begin to identify UX design principles to apply to this tech to increase the acceptance of robots and improve the human-robot interaction experience.

AI benefits from GPU, not CPU advancements
A quick follow-up to our blog posts about AI… The name of the game is no longer Moore's Law where we see processors getting exponentially faster. AI technology is driven not by computing processes of the past, but from an evolution beyond central processing unit (CPU)...

The critical component missing from AI technology
The first step when developing AI is to understand the user need; but just as critical, is knowing the context in which the data is being collected.

Three things to improve acceptance of AI
To truly deliver on the promise of AI, developers need to keep the end users in mind. By integrating three components of context, interaction, and trust, AI can be the runaway success that futurists predict it will be.

Recruiting methods and study logistics for human factors and user research
A stronger recruiting strategy that includes relationships with patient support groups and clinical treatment centers can provide better access to difficult-to-reach patient populations. Being intentional about how you plan the logistics of your human factors and user research can mitigate risks to validity introduced by biases.

Singularity and the potential impact on UX design principles
If we are approaching a rapid technology shift as some experts predict, core UX design principles will have to be redefined to adapt to radically different interaction models.

Am I satisfied or stuck? The impact of ecosystems on household users
Manufacturers building an ecosystem of devices and services should design for both a separate, personalized experience and household or shared experience.

UX and Brand: Delivering on the promise of experience strategy
Bold Insight and The Office of Experience partner to deliver outstanding user experiences.

When designing an experience, are you really thinking about the customer first?
While every organization has constraints to consider when designing experiences for customers or users, designing the ideal customer experience is completely possible within those constraints. Begin by identifying the experience you want your customer to have and work “backward” from there.

UX project logistics: choosing the right vendors for project success
Selecting the correct vendors to support your UX project is critical to success. From facilities to recruiting, knowing the right questions to ask, budget constraints, and client needs and expectations will make the selection process smooth and painless.

Reclassifying diabetes: 3 implications for product design
Recent research suggests that reclassifying diabetes may allow for the development of more targeted diabetes treatments. This could present opportunities to design these treatments to maximize patient safety and experience.

Designing your POS so it’s not a POS
Regardless of whether the interface is intended to be used by a customer (novice) or an employee (expert), the key is to ensure that the POS interface is designed for the intended audience. To do this, organizations should engage users throughout the design process.

FDA’s digital health precertification program emphasizes importance of post-market surveillance
Finding efficient ways to leverage post-market surveillance data to inform product development at an institutional level will be key for SaMD manufacturers seeking FDA precertification.
Confirmation Fatigue: Enough with the reminders already!
While confirmations and reminders are essential and usually well-intentioned, they are annoying. Organizations must uncover if and how their customers will use reminders and confirmations during user testing. Confirms should add to the user experience, not leave users feeling frustrated and tethered.

5 takeaways for human factors practitioners from the HFES Health Care Symposium FDA workshops
Healthcare symposium provides clarity for interpretation of FDA guidance documents related to human factors engineering.

Webisode: Global user research — where to start
Create the conditions to collect highest quality data across diverse environments.




Webisode: Global user research — things to think about
Explore considerations for successful global user research in part two of this three-part webisode series.




Webisode: Why invest in global user research?
While many organizations see the value in user research, there is sometimes a reluctance to invest in a global research program.


In-vehicle UX research: Here’s one recommendation that hasn’t changed in 10 years
I found myself discussing what can be done to increase the extent to which voice recognition systems are seen as a benefit rather than an annoyance with the research sponsors, and I said the same things as I said 10 years ago… improve the system to support and recognize more natural speech patterns.


The future of fan engagement: How do you measure goosebumps?
One of the CES presentations I attended was a panel in the sports technology track called, The Future of Fan Engagement. The panel discussed cutting-edge research in the sports tech market and perspectives on the relationship between emergent media technologies and...


Designing for Voice: The next phase of UX design
Good design involves understanding and incorporating core UX elements (people, environment, and tasks), but frictionless voice UI design needs more: UX designers need to understand the idiosyncrasies of voice as a medium. What we learn, and how those insights are translated into a voice interface design is a new challenge for UX design.


Just in time for the Super Bowl – A football metaphor for UX research and design
User research and user-centered design are inseparable. We are quarterbacks. We don’t like to run.


The time for a better UX in digital therapeutics is now
If history has shown that payer behavior tends to shift once a critical mass has been achieved, and we are on the precipice of achieving that critical mass for digital therapeutics, having a “user friendly solution” is about to replace “having a reimbursable solution” as the #1 factor affecting physician prescribing behavior.
RESEARCH TIPS
Human factors optimization: How to leverage HF researchers in your medtech team
As a medtech professional, you can enhance your team’s capabilities by engaging human factors researchers to create front-end documentation, alleviate research workloads, and provide regulatory guidance.
Enhancing medical device safety and effectiveness: Leveraging knowledge tasks in healthcare UX and human factors research
Discover why implementing knowledge tasks is essential for evaluating user comprehension of critical safety information in medical device validation. Learn how to effectively assess these tasks to enhance product safety and effectiveness in your healthcare UX research.
3 considerations for accessible in-car UX research sessions
Adaptability, alternative setup options, and a prioritized task list are all helpful components to planning in-car research studies for populations with accessibility needs.
IN THE NEWS
Bold Insight and Eli Lilly and Company co-publish journal article on novel assessment tool to enhance medical device usability
Bold Insight team members Kaitlin Stinson, Courtney Roberts, and Stephanie Wiltman recently co-authored a research article with Mikaylah Gross, Senior Principal Human Factors Engineer at Eli Lilly and Company. The article, Improving medical device usability by...
Bold Insight stands out globally as a top workplace for women
This International Women’s Day, The CEO Magazine featured Bold Insight among eight best workplaces in the world for women for its outstanding company culture and policies. The article highlights the industry-leading benefits and perks Bold Insight gives employees and...
Bold Insight to launch AI research project at the 2024 HFES Health Care Symposium
This month, Bold Insight team members will attend and present at the Human Factors and Ergonomics Society (HFES) 2024 Symposium. The event will connect professionals including human factors experts, pharmaceutical and medical device companies, biomedical engineers,...